Kaua’i doctor shortage includes most specialities, forcing residents to fly to O’ahu
There is no endocrinologist on the Garden Isle. No out-patient neurologist. No oncologist. No psychologist or ophthalmologist that is accepting new patients. Specialists in rheumatology and gerontology also are nonexistent.
Jim Winkler, founder of Hale Lea Medicine & Urgent Care Clinic in Kīlauea on Kauaʻi, recited this list of empty local healthcare positions in a viral video uploaded to TikTok last month.

“The human face of this [shortage] is profound,” Winker, a certified physician’s assistant, said in the 48-second clip set to melancholy piano music.
“These are patients who are depressed, suicidal, have breast cancer, ovarian cancer, diabetes, hypertension. These are our aunties and uncles. These are our children.”
Kaua‘i is short 43 full-time physicians (26%), part of the 732 full-time physicians or equivalents needed statewide, according to the 2022 Physician Workforce Report issued to the state legislature. Hawai’i County is down 187 full-time physicians (40%) and Maui County is short 158 full-time physicians (40%).
A 2021 NursingEducation analysis determined Kaua‘i County had the 13th-largest shortage of healthcare workers in the United States. Hawai‘i County had the third-largest shortage and Maui County had the fifth-largest.
This month, a study found 75% of Hawai‘i’s rural hospitals are at immediate risk of closure.
“I haven’t taken a salary in four months, just to keep the facility going,” Winkler said in another TikTok video, recorded at the same Grassroot Institute of Hawai‘i-sponsored event on O‘ahu.
“Our facility is a canary in the coal mine, but we’re one of many canaries. There are canaries dropping out everyday. We’ve lost 25% of our private practices in Hawai‘i in the last two years.”
The Grassroot Institute is a conservative think tank advocating for the exemption of medical services from Hawai‘i’s general excise tax. Such a move, intended to alleviate the state’s doctor shortage, is supported by newly-elected Democratic governor and physician Josh Green, who up until recently practiced on the Big Island.
A bipartisan group of state senators introduced a bill that would have exempted medical services from the GET in 2021. But the legislation, which also exempted food and hygiene products, went nowhere.
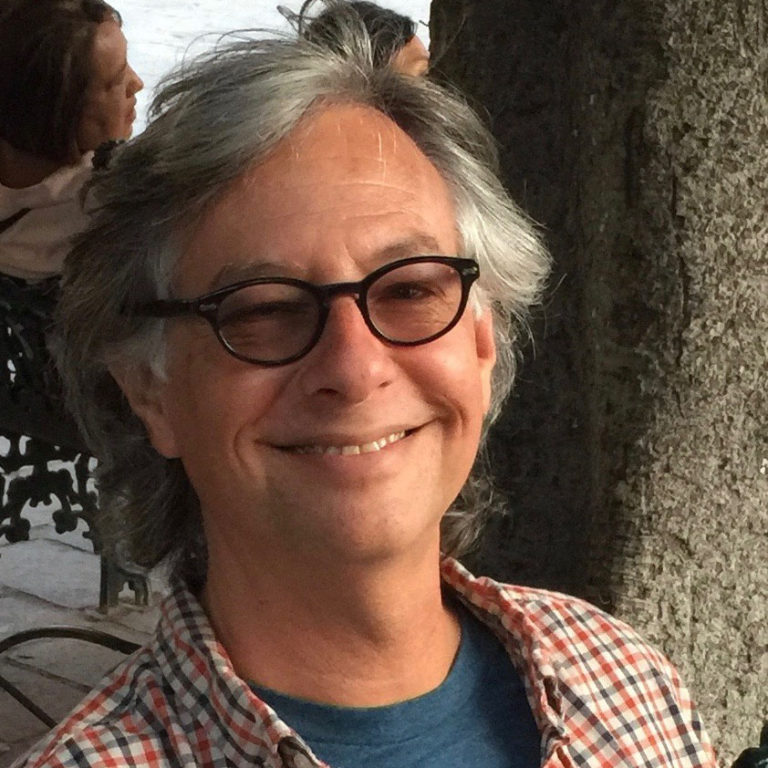
The Grassroot Institute’s TikTok videos of Winkler have racked up more than 725,000 views. But nothing has changed, he wrote in an email to Kaua‘i Now.
“Recruiting and retaining healthcare workers is a nightmare – Physicians, PAs, NPs, physical therapists, nurses. Inadequate insurance reimbursement from HMSA [Hawaiʻi Medical Service Association], Medicare and Quest means insufficient salaries for healthcare workers to live in Hawai‘i,” Winkler explained.
“Statistics confirm that Neighbor Islands have higher death rates from many causes due to the lack of healthcare providers. In plain English – you’re more likely to die if you live on Kaua‘i, Big Island or Maui than on O‘ahu.”
Dr. Avery Creech, Kaua‘i’s only audiologist, is one of the relatively few medical specialists now working on the island. She’s seen her already-niche field shrink since the beginning of the coronavirus pandemic, when other practices with advanced equipment halted local appointments.
“Those other practices stopped coming to Kaua‘i for different reasons, whether it was illness, or someone passed away, or it just wasn’t financially feasible,” Creech said.
The off-island specialists had provided audiological care for all patients under the age of 7. But Creech’s clinic, Island Audiology in Līhu‘e, was unable to immediately plug the gaps in service created by their departure. This meant young patients could only be seen at a specialty clinic on O‘ahu.
“That leaves that opportunity for children to fall through the cracks,” Creech said.
She explained off-island care can be delayed by families who need to wait for a good time to travel, or for their insurance provider to approve the trip. Sometimes, the health concern requiring the trip is neglected completely.
Island Audiology has since begun to add the technology needed to provide care for Kaua‘i’s small children and babies.

“When you have hearing loss as a child and it’s not being treated appropriately, it has bigger implications throughout your life the longer that it goes on,” Creech said.
“It’s these little things that, in the grand scheme of things, it’s hard to know exactly what to do with. But in the meantime, while we’re trying to figure all this out as health care providers on the island, there’s actual people paying a price.”
Dayna Manglallan, a children’s services specialist at the YWCA of Kaua‘i, is one such person. She was medevaced to O‘ahu following pregnancy complications in August.
“If something was wrong with the baby, they wouldn’t have had the right tools to take care of her,” Manglallan said while cradling her now 3-month-old daughter.
The 3 a.m. flight cost more than $80,000, although Manglallan’s insurance covered the vast majority of the hefty bill.
“I still have bills coming in, from the EMS from KVMH [Kaua‘i Veterans Memorial Hospital] to Līhu‘e, then the medivac, then the ambulance from Honolulu to Kapiolani [Medical Center],” Manglallan said.
“It was a lot and it was very overwhelming.”
But there is a new program in the works to tackle the island’s doctor shortage. The University of Hawaiʻi at Mānoa’s John A. Burns School of Medicine (JABSOM) announced the Kaua‘i Medical Training Track in March. The program is being funded with a six-year, $10 million commitment by billionaire couple Dr. Priscilla Chan and Facebook founder Mark Zuckerberg, who own large swaths of Kaua‘i’s North Shore.
The initiative begins next spring, when its first six students start their initial residency on Kaua‘i, according to Dr. Travis Hong, the medical school’s Director of Rural Training.
“Historically, JABSOM has always had students centric to O‘ahu,” said Hong, explaining most students only receive opportunities to train on the Neighbor Islands in their last two years of study.
“This is the first actual parallel track in the medical school’s history where it’s just for Kaua‘i. These six students are going to be basically spending significantly more time on Kaua‘i than they would have if they had gone through traditional routes.”
Students accepted into the program receive full scholarships after committing to practice on Kaua‘i for at least four years post-graduation.
Hong, who lives and works on O‘ahu, was born and raised on Kaua‘i. He remembers full-page ads published in the island’s local newspaper, welcoming newly-arrived physicians to the community.
“And six months later, they were gone. You’re thinking, ‘What happened?’” Hong chuckled ruefully.
Hong, like Winkler, points to Kaua‘i’s high cost of living as a key reason behind its health care shortage.
The island’s remote geography is another one of the many other factors at play. Transplant physicians can find themselves called back to the U.S. mainland or elsewhere at any time, for any number of reasons.
“It’s a transition to live on Kaua‘i,” Hong said. “It may not be for everyone. Whether it’s the lifestyle, or … people start having children and then it’s tough to find childcare or good educational resources, or they have family they need to go back to. It’s tough.”
Hong and others have found doctors who make it long-term on Kaua‘i are greatly attached to the island and its people, often through family bonds — or love of surfing on uncrowded beaches, Hong jokes. Therefore, the Kaua‘i Medical Training Track gives preference to applicants with strong local connections.
He hopes the program becomes a blueprint for Hawai‘i’s other Neighbor Islands.
“I really believe it’s gonna be successful. I think we’re addressing a great need for Kaua‘i,” he said. “I hope 10 years down the line, the program’s still going and getting that pipeline for new health care providers.”
Sponsored Content
Comments



_1770333123096.webp)